Is There A Test That The Department Of Health Can Test Animal Blood
Contact the Rabies Unit
The Rabies Unit is open up from 9:00am to 5:00pm, Monday through Fri. It is closed on weekends and holidays.
rabies.PHEL@doh.nj.gov
(609) 530-8416hotline
For emergency rabies testing, contact the Communicable Disease Service Rabies Atomic number 82 at 609-826-4871 or 609-826-4882.
Did you know?
- The PHEL Rabies Unit tests nigh 3,000 animals each year
- Rabies occurs near often in wild animals
- Among domestic animals, cats are the nigh often positive
- Wild fauna tested include raccoons, bats, skunks, groundhogs and foxes
- Among wildlife, raccoons are near often positive for rabies
- Fewer than 1 percent (1%) of bats carry rabies in New Jersey
- PHEL tests livestock and domesticated wildlife
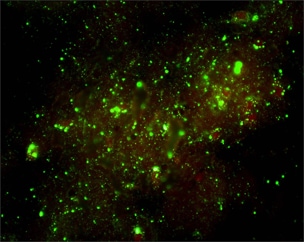
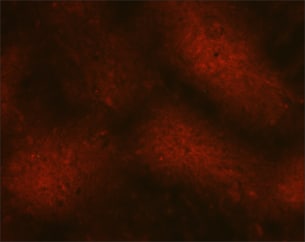
- The test for rabies is performed on fauna brain tissue
- PHEL utilizes the Direct Fluorescent Antibody (DFA) method
- Rabies testing follows the CDC standardized testing protocol
- Highly trained laboratory personnel perform rabies testing
- Testing is done nether strict bioSafety standards
- Sample handling and disposal follows WHO/CDC Standards
Rabies Testing
How do I...?
How can we assistance y'all today?
- 0 Web Pages
- 0 Wellness Facilities
- 0 Job Openings
Last Reviewed: vi/15/2015
Most the New Jersey Section of Wellness
Final Reviewed: i/3/2019
Your Wellness
Last Reviewed: 12/15/2018
Healthcare Facilities & Services

New Jersey is home to over 2,000 licensed hospitals, nursing homes, and medical intendance facilities. The New Bailiwick of jersey Section of Health works to ensure that citizens receive advisable levels of care in every regulated facility.
Last Reviewed: 3/six/2019
Public Health
Terminal Reviewed: 5/30/2019
Health IT, Facts & Findings
Last Reviewed: 12/19/2017
Source: https://www.nj.gov/health/phel/public-health-lab-testing/rabies
Posted by: bowleytroses.blogspot.com

0 Response to "Is There A Test That The Department Of Health Can Test Animal Blood"
Post a Comment